The landscape of clinical trials is continually evolving to accommodate the complexities of modern drug development. Within this dynamic environment, risk-based monitoring (RBM) has emerged as a pivotal strategy to enhance the efficiency and effectiveness of clinical trials. By focusing on critical data points and adaptive methodologies, RBM enables researchers to navigate the inherent uncertainties of clinical studies. This article explores the impact of RBM on clinical trial design, decision-making, and the integration of real-world data, particularly in the context of oncology and precision medicine.
Key Takeaways
- Risk-based monitoring is crucial for optimizing resource allocation in clinical trials, ensuring patient safety, and maintaining protocol compliance.
- Strategic use of Monte Carlo simulations and adaptive trial designs can significantly reduce uncertainty in clinical trial outcomes.
- Advanced analytics and independent randomization centers play a vital role in improving decision-making and trial efficiency.
- Integrating real-world data and evidence is essential for bridging the gap between randomized control trials and practical clinical applications in oncology.
- Innovative trial designs, particularly those adaptive to biomarker-driven treatments, are advancing the field of precision medicine and de-risking drug development.
The Evolution of Risk-Based Monitoring in Clinical Trials

Historical Perspective and Regulatory Endorsement
The inception of risk-based monitoring (RBM) in clinical trials marks a significant shift from traditional monitoring approaches. Initially, clinical trial oversight was heavily reliant on frequent on-site visits and source data verification, which often led to inefficiencies and increased costs. The evolution towards RBM was driven by the need to enhance trial efficiency and data quality, while also ensuring patient safety.
Regulatory bodies, recognizing the potential of RBM, have endorsed its use through various guidelines. The FDA’s guidance on a risk-based approach to monitoring, along with similar recommendations from the EMA and ICH, underscores the global shift towards more strategic trial oversight. These endorsements have paved the way for the integration of advanced statistical methods, such as Bayesian models and statistical process control, into the monitoring process.
The strategic implementation of RBM is not without challenges, yet it offers a framework for more focused and effective monitoring. By prioritizing high-risk areas and utilizing predictive analytics, RBM aims to preemptively address issues before they escalate.
The table below highlights key regulatory milestones that have endorsed RBM:
| Year | Regulatory Body | Milestone |
|---|---|---|
| 2013 | FDA | Guidance on RBM |
| 2016 | EMA | Reflection on RBM |
| 2018 | ICH | Revision of Guidelines |
As the industry continues to navigate the complexities of clinical trial monitoring, the historical perspective provides a foundation for understanding the current landscape and the regulatory support that has shaped it.
Key Components and Strategic Implementation
The strategic implementation of Risk-Based Monitoring (RBM) is pivotal in modernizing clinical trial oversight. It requires a clear framework that aligns with the overarching goals of ensuring data quality and participant safety. At the core of RBM lies the necessity to identify and mitigate risks throughout the trial lifecycle. This involves a continuous process of risk assessment, the establishment of key risk indicators, and the application of central data monitoring techniques.
To effectively implement RBM, organizations must adopt an Agile, Collaborative, Efficient (ACE) approach. This ensures that teams are prepared to handle the dynamic nature of clinical trials and can adapt to emerging data and risks. The integration of technology solutions is also crucial, as they provide the infrastructure for central monitoring and data analysis. A successful RBM strategy hinges on the ability to customize these solutions to meet specific trial requirements while maintaining a solid product roadmap.
The essence of strategic implementation in RBM is not just in adopting new methods, but in fostering a culture of quality and efficiency that permeates every aspect of the trial.
Ultimately, the goal is to empower trial leaders with the tools and insights needed to make informed decisions, secure necessary resources, and enhance business capabilities. This empowerment is the cornerstone of a robust RBM system that can navigate the complexities of clinical trials and ensure a seamless transition for teams.
Challenges and Solutions in Clinical Trial Site Monitoring
Clinical Trial Site Monitoring is a pivotal aspect of risk-based monitoring (RBM), demanding timely insights generation from site data to ensure patient safety and protocol adherence. The FDA and EMA have strongly endorsed RBM, emphasizing its strategic role in resource allocation based on critical indicators such as data criticality and patient safety.
Key challenges in site monitoring include the need for real-time data analysis, the scarcity of trained research personnel, and constraints on in-person site inspections. To address these issues, the industry is increasingly turning to remote site monitoring technologies. These include centralized monitoring and data visualization dashboards, which facilitate oversight while reducing the need for physical site visits.
The adoption of remote monitoring technologies represents a paradigm shift in clinical trial oversight, enabling more efficient and effective monitoring practices.
Solutions to these challenges also involve leveraging commercial and open-source software for innovative trial design, and focusing on formal interim analyses to reduce independent data monitoring committee timelines.
Optimizing Clinical Trial Design Amidst Uncertainty

Incorporating Monte Carlo Simulations for Strategic Planning
Monte Carlo simulations have become an indispensable tool in the strategic planning of clinical trials. At its core, Monte Carlo simulation is a computational technique used to approximate the probability of outcomes by running a large number of simulations. This method allows for the exploration of various trial designs and the assessment of their robustness against the inherent uncertainties of clinical research.
The power of Monte Carlo simulations lies in their ability to model complex systems and to provide a distribution of possible outcomes rather than a single deterministic prediction. By simulating thousands of trial scenarios, researchers can identify the most promising trial designs before actual implementation. This approach not only saves time and resources but also enhances the probability of trial success.
The strategic use of Monte Carlo simulations can lead to more informed decision-making, optimizing both the design and the conduct of clinical trials.
For instance, simulations can be used to determine the optimal timing for interim analyses, a critical component of adaptive trial designs. They can also help in forecasting patient enrollment rates, which is crucial for maintaining trial timelines. Below is a list of key applications of Monte Carlo simulations in clinical trial planning:
- Assessing the impact of different trial parameters on outcomes
- Estimating the probability of trial success under various scenarios
- Optimizing the number and timing of interim analyses
- Forecasting patient enrollment and retention rates
- Evaluating the potential for adaptive trial designs
Adaptive Designs: Flexibility and Case Studies
Adaptive designs in clinical trials have revolutionized the way researchers approach uncertainty and change within studies. These designs allow for modifications to the trial or statistical procedures as data accumulates, enhancing the ability to respond to emerging trends and evidence. This flexibility is particularly beneficial in the context of precision medicine, where treatments can be tailored to individual patient responses.
Diversity in clinical trials is a critical factor that adaptive designs can address effectively. By incorporating a range of patient populations and allowing for adjustments based on interim data, these trials can become more inclusive and representative. The table below outlines key aspects of adaptive designs that contribute to this diversity:
| Aspect | Description |
|---|---|
| Inclusivity | Broadening eligibility criteria to include diverse populations |
| Interim Analysis | Adjusting strategies based on early results |
| Response-Adaptive Randomization | Allocating more patients to better-performing treatments |
Adaptive designs not only offer a methodological advantage but also an ethical one, as they can reduce patient exposure to less effective treatments and potentially shorten the time to market for beneficial therapies.
Case studies have demonstrated the success of adaptive designs in various therapeutic areas. For instance, platform trials, which are a type of adaptive trial, have been noted for their flexibility and adaptability, allowing for dynamic adjustments based on accumulating evidence. These trials exemplify the evolution of clinical trial design, where the focus is on learning and adapting rather than merely confirming preconceived hypotheses.
Multi-Arm Multi-Stage Trials: Design and Monitoring Considerations
Multi-Arm Multi-Stage (MAMS) trials represent a significant advancement in the strategic planning of clinical studies. These designs allow for interim analyses to assess multiple treatments simultaneously, providing a more efficient pathway to identifying effective therapies. MAMS trials are particularly beneficial in scenarios where there are several promising candidates, as they can reduce the overall sample size required and potentially accelerate the drug development process.
Key considerations in MAMS trial design include the determination of stopping rules, interim analysis schedules, and criteria for dropping ineffective arms. The following table outlines the essential parameters for optimizing MAMS designs:
| Parameter | Description |
|---|---|
| Stopping Rules | Criteria for terminating an arm early due to lack of efficacy or safety concerns. |
| Interim Analysis | Scheduled assessments to evaluate ongoing trial data. |
| Treatment Selection | Process for choosing which treatments continue to the next stage. |
| Sample Size Re-estimation | Adjustments to the number of participants based on interim results. |
By carefully calibrating these parameters, researchers can navigate the inherent uncertainties of clinical trials while maximizing the potential for successful outcomes.
The implementation of MAMS designs also requires robust statistical programming and data management systems to handle the complexity of the data and analysis. It is crucial to have a clear operational plan that addresses the logistical challenges of conducting a trial with multiple arms and stages.
Enhancing Decision-Making and Efficiency in Clinical Trials

Improving Go/No-Go Decisions with Advanced Analytics
The integration of advanced analytics into the decision-making process of clinical trials has marked a significant shift towards more data-driven outcomes. Advanced analytics tools enable a more nuanced analysis of trial data, leading to improved go/no-go decisions that are critical to the progression of clinical studies.
- Predictive Modeling: Utilizes historical data and current trial metrics to forecast outcomes.
- Simulation Techniques: Assess trial design and decision rules under various scenarios.
- Bayesian Methods: Provide a probabilistic framework for decision-making.
The use of advanced analytics not only enhances the accuracy of decisions but also reduces the time and cost associated with lengthy trial periods.
Incorporating these tools requires a strategic approach, ensuring that the data is not only collected but also interpreted correctly. The ultimate goal is to minimize risk and maximize the potential for successful trial outcomes.
Statistical Programming: Impact on Management and Outputs
The synergy between statisticians and programmers is pivotal in the realm of clinical trials. Effective communication is the cornerstone of this relationship, ensuring that complex statistical models are accurately implemented and efficacy outputs are efficiently produced. Programmers are tasked with creating Analysis Data Models (ADaMs) that adhere to CDISC standards, a process that is intricate and demands precision.
In the context of statistical programming, the creation of multicell dot plots, the use of functions like Proc Fcmp, and the development of data validation tools using R Shiny exemplify the diverse skill set required. The challenge of optimizing listings and tables further underscores the need for meticulous attention to detail, as variations in data length and categorical values can significantly impact the presentation and usability of trial data.
The integration of multiple programming languages within a single platform presents both opportunities and challenges. Strategies to enhance the user experience for statistical programming teams are essential for the successful management and output of clinical trial data.
The table below illustrates the comparison of programming approaches in statistical programming:
| Reference | Comparison Aspect | SAS Approach | R Approach |
|---|---|---|---|
| PO-196 | Multicell Dot Plots | Traditional | Innovative |
| PO-231 | Function Usage | Proc Fcmp | Equivalent R Function |
| PO-258 | Data Validation | Not Specified | R Shiny Tool |
Understanding the nuances of these programming challenges and the tools available is crucial for the advancement of clinical trial methodologies and the achievement of robust, reliable results.
The Role of Independent Randomization Centers
Independent randomization centers play a pivotal role in preserving the integrity of clinical trials by ensuring unbiased allocation of participants to different study arms. Their involvement is crucial in maintaining the scientific validity of the trial outcomes.
Randomization centers are responsible for implementing the randomization method, which includes generating random allocation sequences and securely providing them to investigators. This process minimizes selection and confounding biases, which are potential threats to the validity of a study.
In scenarios where unblinding is necessary, such as for IND safety reporting or interim analyses, the randomization center must ensure that the integrity of the blinding is maintained to the greatest extent possible.
The table below outlines the key functions of an independent randomization center:
| Function | Description |
|---|---|
| Sequence Generation | Creating a random and unpredictable allocation sequence. |
| Allocation Concealment | Ensuring the sequence is not disclosed before assignment. |
| Implementation | Providing the sequence to investigators in a secure manner. |
| Unblinding Management | Safeguarding the blinding during necessary unblinding events. |
Integrating Real-World Data and Evidence in Oncology Trials

Bridging the Gap Between RCTs and Real-World Data
The integration of real-world data (RWD) with randomized control trials (RCTs) is a pivotal step in enhancing the applicability of clinical research findings to everyday clinical practice. While RCTs are renowned for their rigorous methodology and control, they often operate in a somewhat artificial environment that may not fully represent the patient population at large.
To address this, researchers are increasingly looking to RWD to complement and extend the insights gained from RCTs. This synergy allows for a more nuanced understanding of treatment effectiveness and safety in a real-world setting. For instance, RWD can provide valuable information on long-term outcomes, rare side effects, and patient-reported outcomes that are not typically captured in the controlled setting of an RCT.
The challenge lies in ensuring the fit-for-use quality of RWD, which necessitates stringent criteria for data accuracy and completeness. This is essential for the data to be reliable and for the evidence to be considered robust enough to inform clinical and regulatory decisions.
The table below outlines the key considerations when evaluating the fit-for-use quality of oncology RWD:
| Consideration | Description |
|---|---|
| Data Source | Origin of data, such as EMRs, patient registries, or claims databases. |
| Data Completeness | Extent to which all relevant data points are captured. |
| Data Accuracy | Precision and correctness of the data collected. |
| Patient Representativeness | How well the data reflects the broader patient population. |
| Outcome Relevance | The degree to which the data captures outcomes that matter to patients and clinicians. |
By meticulously evaluating these aspects, researchers can bridge the gap between the controlled environment of RCTs and the diverse landscape of real-world clinical practice.
The Fundamentals of Real World Evidence in Drug Development
Real world evidence (RWE) has become a cornerstone in the landscape of clinical research, offering a wealth of insights into drug safety, effectiveness, and patient outcomes. The integration of RWE into clinical trial frameworks is revolutionizing the way we understand and evaluate medical interventions.
The FDA’s endorsement of RWE for regulatory decision-making underscores its significance. Particularly, the use of RWE as a control arm in clinical trials presents a unique opportunity to enhance study designs while addressing common recruitment challenges.
The strategic use of real-world data can streamline the development process, providing a robust alternative to traditional randomized control trials (RCTs).
The following table highlights the key areas where RWE is making an impact in clinical research:
| Area of Impact | Description |
|---|---|
| Personalized Medicine | Tailoring treatments based on patient-specific data. |
| Patient Recruitment | Improving efficiency and effectiveness. |
| Treatment Effectiveness | Assessing real-world outcomes. |
| Post-approval Safety | Monitoring long-term safety and efficacy. |
As the adoption of RWE solutions continues to grow, clinical trial management systems (CTMS) are evolving to support the collection and analysis of this data, ensuring its accuracy and completeness.
Case Study: Redesigning a Pragmatic Trial in Oncology
The redesign of a pragmatic trial in oncology can be a complex endeavor, particularly when aiming to improve health outcomes for marginalized people. This case study illustrates the strategic adjustments made to an existing trial framework to better address the unique needs of this population. The modifications included:
- A more inclusive patient recruitment strategy to ensure diverse representation.
- Enhanced data collection methods to capture relevant social determinants of health.
- Implementation of patient-centric endpoints that resonate with the lived experiences of the participants.
The focus on marginalized groups not only enriches the data but also aligns the trial outcomes with broader public health goals.
The results of these changes were promising, showing an increase in patient engagement and a more comprehensive understanding of treatment effects across different subpopulations. The table below summarizes the key metrics before and after the redesign:
| Metric | Pre-Redesign | Post-Redesign |
|---|---|---|
| Patient Recruitment Rate | 60% | 85% |
| Diversity of Participants | Low | High |
| Data Completeness | 70% | 95% |
By prioritizing inclusivity and patient relevance, the trial not only became more ethical but also gained in scientific rigor, potentially leading to more accurate and generalizable findings.
Advancing Precision Medicine with Innovative Trial Designs

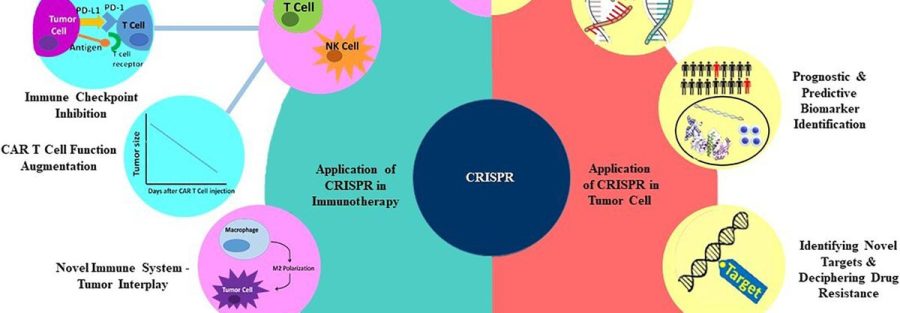
Adaptive Designs for Biomarker-Driven Treatments
The integration of biomarkers in clinical trial design has revolutionized the approach to oncology drug development. Adaptive designs tailored for biomarker-driven treatments allow for dynamic adjustments based on real-time data, enhancing the precision of therapeutic interventions. These designs facilitate the identification of patient subgroups that are most likely to benefit from a specific treatment, thereby improving the overall success rates of clinical trials.
In the context of biomarker-driven trials, population enrichment strategies are critical. They involve selecting a patient population with a higher likelihood of responding to the treatment based on predictive biomarkers. This approach not only increases the probability of clinical success but also ensures a more efficient use of resources.
The ability to adapt trial protocols in response to interim results can significantly de-risk drug development, providing a pathway to more personalized healthcare solutions.
The table below outlines the key benefits of adaptive designs in biomarker-driven treatments:
| Benefit | Description |
|---|---|
| Enhanced Efficacy | Targeting patient subgroups likely to respond. |
| Reduced Costs | Avoiding treatment of non-responders. |
| Faster Decisions | Interim analyses lead to quicker adaptations. |
| Regulatory Support | Agencies encourage designs that improve trial efficiency. |
Adaptive designs are not without challenges; however, the industry is witnessing a shift towards more flexible and innovative approaches to clinical trial design, as evidenced by the increasing number of trials incorporating these methods.
Utilizing Historical Data to Mitigate Clinical Trial Risks
In the realm of clinical trials, historical data serves as a crucial asset for enhancing study design and reducing risk. By analyzing past trials, researchers can identify patterns and outcomes that inform the planning of new studies, ensuring more robust and efficient trial designs. This retrospective analysis can be particularly valuable in rare disease research, where patient populations are limited and every data point is vital.
Historical data can also be used to create synthetic control arms, providing a comparison group without the need for additional patient enrollment. This approach not only saves time and resources but also reduces patient exposure to potentially less effective treatments.
The integration of historical data is not without challenges; however, it is a powerful tool for preserving trial integrity and enhancing data quality.
The table below outlines key aspects of utilizing historical data in clinical trial design:
| Aspect | Description |
|---|---|
| Recruitment Efficiency | Improves by predicting enrollment rates and identifying potential hurdles. |
| Study Sample Optimization | Enhances by understanding the variability within historical patient populations. |
| Control Arm Construction | Facilitates through the use of existing data to form synthetic or external control arms. |
| Bias Mitigation | Aids by recognizing and adjusting for biases present in past studies. |
Embracing historical data is a step towards diversity in clinical trial data transparency, fostering an environment where trials are not only more efficient but also more representative and reliable.
De-risking Drug Development with Adaptive Design Strategies
Adaptive design strategies in clinical trials offer a dynamic approach to drug development, allowing for modifications to the trial or statistical procedures as data accumulates. These strategies can significantly reduce the risk and cost associated with drug development by enabling more efficient decision-making processes.
One of the key advantages of adaptive designs is their ability to address uncertainties in clinical trials. For instance, the VALOR trial utilized a promising zone design, enhancing the probability of success for Vosaroxin, a treatment candidate. Similarly, Bayesian dose-escalation methods have been refreshed to improve model-based algorithms for Phase I trials.
Adaptive designs are not without challenges, however. The FDA’s 2010 draft guidance on adaptive design clinical trials highlights the complexities involved in less well-understood adaptive methods. To navigate these challenges, it is crucial to consider the following steps before implementing an adaptive design:
- Understand the specific objectives and endpoints of the trial.
- Determine the potential adaptations that may be required.
- Assess the statistical implications of proposed adaptations.
- Ensure clear communication with regulatory authorities.
By embracing adaptive design strategies, drug developers can make more informed decisions, optimize resource allocation, and potentially bring effective treatments to patients more quickly.
Conclusion
Risk-based monitoring (RBM) has emerged as a pivotal strategy in the conduct of clinical trials, addressing the inherent uncertainties and optimizing resource allocation. Endorsed by regulatory authorities such as the FDA and EMA, RBM facilitates a more strategic oversight of clinical investigations, focusing on critical data, patient safety, and protocol adherence. Articles and case studies highlight the evolution of RBM, showcasing its integration with adaptive designs, the use of real-world evidence, and the importance of robust decision-making processes. As the landscape of drug development continues to evolve, RBM stands as a testament to the industry’s commitment to innovation, efficiency, and, most importantly, patient welfare. The collective insights from various publications underscore the necessity for continuous improvement and adaptation in monitoring practices to ensure the successful execution and completion of clinical trials.
Frequently Asked Questions
What is risk-based monitoring (RBM) in clinical trials?
Risk-based monitoring (RBM) is a strategic approach to monitoring clinical trials that focuses on identifying, assessing, and prioritizing risks to patient safety and data integrity. It involves allocating monitoring resources where they are most needed, based on key indicators such as data criticality, patient safety, and protocol compliance.
How has the FDA and EMA endorsed risk-based monitoring?
Both the FDA and EMA have strongly endorsed risk-based monitoring as an efficient way to oversee clinical investigations. They encourage sponsors to adopt RBM practices to enhance trial oversight and ensure the protection of trial participants while maintaining data quality.
What are some challenges in clinical trial site monitoring?
Challenges in clinical trial site monitoring include ensuring consistent protocol adherence, managing diverse data sources, maintaining data quality, dealing with variable site performance, and adapting to remote monitoring requirements, especially in the context of RBM.
How do adaptive designs contribute to clinical trial optimization?
Adaptive designs offer flexibility to modify trial parameters based on interim data analysis. This allows for more efficient use of resources, potential early trial termination if results are conclusive, and the ability to adjust the study in response to unexpected findings, ultimately leading to more robust and efficient trials.
What role does real-world data play in oncology trials?
Real-world data (RWD) bridges the gap between randomized control trials (RCTs) and actual clinical practice by providing insights into drug uptake and safety in broader patient populations. RWD can inform trial design, support regulatory decisions, and help assess the generalizability of trial results.
What is the significance of multi-arm multi-stage (MAMS) trials?
Multi-arm multi-stage (MAMS) trials allow for the simultaneous comparison of several treatments against a common control, with the ability to stop arms for futility or declare success at interim stages. This design increases efficiency by reducing the number of patients and time needed to evaluate multiple treatments.